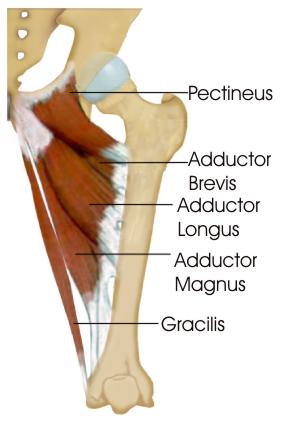
A recently published article by Haroy et al, in the British Journal of Sports Medicine, described a simple exercise routine that decreased the number of groin injuries in male footballers by 41%. Groin injuries are very common in football. Research shows that weaker groin muscles are associated with an increased risk of groin muscle injury. So strengthening groin muscles can potentially prevent injury. The paper studied the Copenhagen Adduction exercise, which has previously been shown to strongly recruit adductor longus. Haroy et al, offered the Copenhagen at three levels of resistance, based on the players’ pain. Players started with Level 3. If the exercise gave them more than 3/10 pain, they were instructed to do the exercise level below instead: 3 > 2 > 1.
The training protocol is shown in the following table: Being only one, quick exercise, compliance was high. They found performing the Copenhagens decreased the risk of groin injury by 41%.
The full article is HERE. Copenhagens are definitely worth adding to your training. The concept is similar to strengthening hamstrings with the Nordic Hamstring Curl which has been shown to prevent 70%-85% of hamstring strain injuries.
HEEL PAIN IN CHILDREN
Sever’s is most common in 9 - 12 year olds. It’s sore to squeeze the bone at the base of the Achilles where it attaches onto the heel. It’s not something that can be seen - it never seems to look red or swollen. It’s worse after sprinting, jumping, and hopping. It settles with rest. It is an overuse injury so it’s common in pre-season, or anytime training loads increase too quickly. My kids get it when they do extra sessions in running spikes or footy boots, without the normal heel support of their running shoes. It’s an overuse injury from excessive loads.
OVERUSE INJURY
When we talk about excessive loads it can be “external” load such as:
I think the running pace is the more powerful multiplier in this list. Extra sprint sessions will do it. My kids got sore once when we did a boot-camp session with a novel plyometric exercise - split jumps. There are also “internal” variables that determine our ability to cope with the training load:
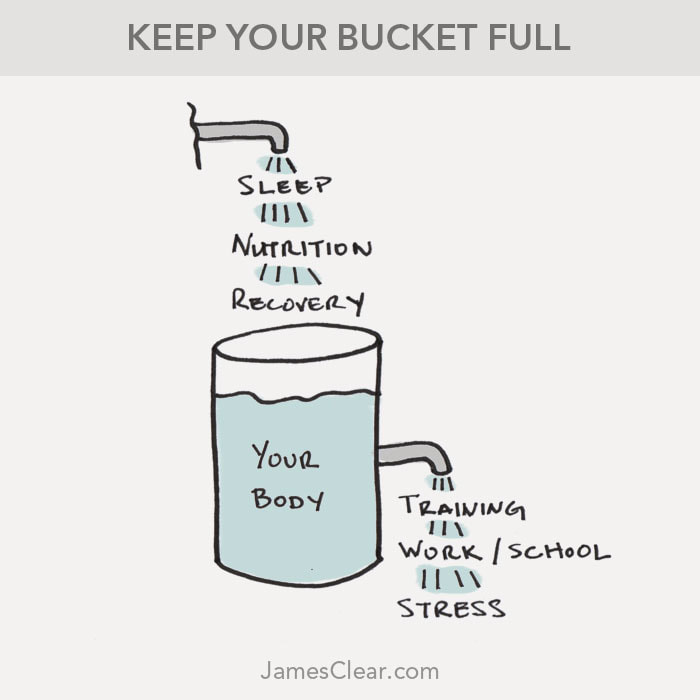
My kids definitely are more prone to Sever’s if they’ve had a couple of late nights that week. And, if they’re having a growth spurt, their bodies are busy spending resources on growing rather than recovering from the stress of a training session. NATURAL RECOVERY
Text books say that Sever’s disease is self-limiting because the growth plate eventually fuses by the age of 15 or 16. But I don’t think there’s anyone who would be happy to just let it run its course until then. It is usually sore enough to stop you participating in sport, so it needs treatment.
WHAT DO WE DO?
I used to put kids with heel pain in orthotics, until I read this research which confirms that a simple heel wedge is more effective than orthotics for Sever’s disease.
I get them to do an isometric Achilles strengthening program which also helps with pain control. But ultimately recovery comes down to load management. Load management means reducing the excessive loads. So this could be:
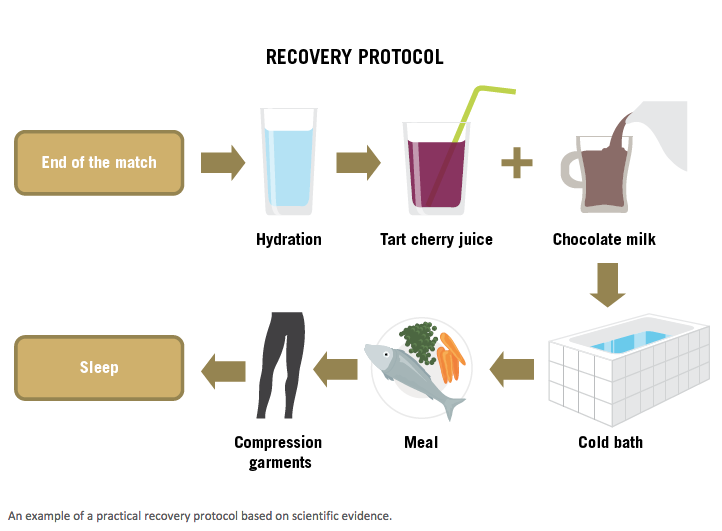
And aid recovery with:
With these type of overuse injuries, I interpret "soreness" as essentially the same thing as "tiredness". If they've been training more, sleeping less, or growing more, we would expect some "tiredness". If they were tired what would be the treatment?... Sleep more and train a bit less.
Summary of:
FOOTBALL RECOVERY STRATEGIES (Grégory Dupont, Mathieu Nédélec, Alan McCall, Serge Berthoin and Nicola A. Maffiuletti, 2015) Does Fatigue Cause injury?
|
| Often when I’m talking to my patient about their injury and why it has happened, they guiltily report that they don’t stretch enough. We’ve all grown up being told how important is it to stretch:
|
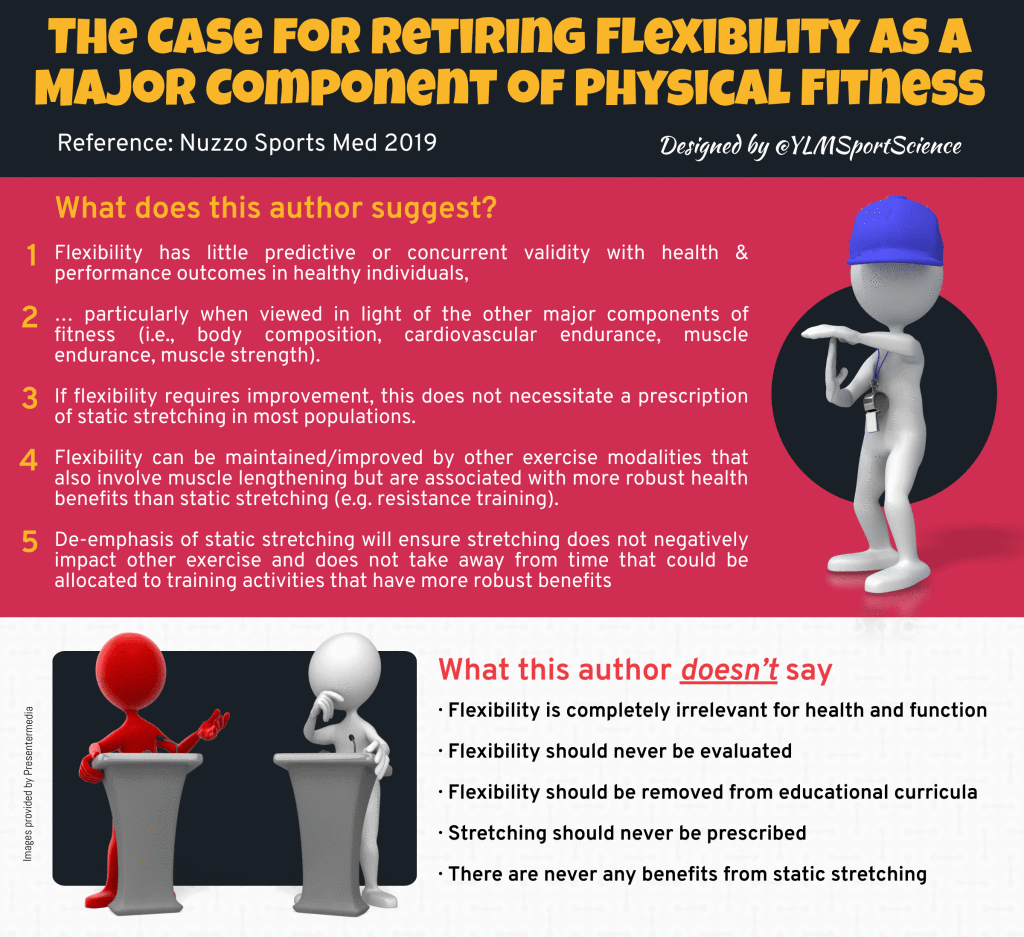
Interestingly, health professionals have changed our tune about the importance of stretching. Research over the last 15 years has suggested static stretching is not as beneficial as was once thought. I’ve been having conversations about the reasons to stretch (or not) for at least the last 15 years, but the current science on stretching just isn’t catching on.
So, what do we know?…
DOES STRETCHING PREVENT INJURIES?
Therefore, in practical terms the average athlete would need to stretch for 23 years to prevent one injury. Definitely not worth it.
DOES STRETCHING HELP MUSCLE SORENESS?
DOES STRETCHING INCREASE RANGE OF MOVEMENT?
DOES STRETCHING HELP PERFORMANCE?
A substantial body of research has shown that sustained static stretching acutely decreases muscle strength and power (ref). Stretching before an endurance event lowers endurance performance and increases the energy cost of running (ref). Cycling efficiency and time to exhaustion are reduced after static stretching (ref).
Pretty much any measure of performance is made worse by stretching. Static stretching impairs:
- strength
- maximal voluntary contraction
- isometric force
- isokinetic torque
- one repetition maximum lifts
- power
- vertical jump
- sprint times
- running economy
- agility
- balance
A comprehensive review (ref) from 2011 concludes:
WHAT ABOUT DYNAMIC STRETCHING?
SO WHY STRETCH?
SO SHOULD WE STOP STRETCHING?
- Will introducing independent doctors at games help the AFL tackle its concussion problem? -
- The unstoppable rise of the carbon-fibre super shoe -
- Muscle building and resistance training often get ignored, but they're likely to help us age better -
- Evidence doesn't support spinal cord stimulators for chronic back pain -
- Surgery won't fix my chronic back pain, so what will? -
- Can a good night's sleep protect collision sport athletes against concussion? -
- Beetroot isn't vegetable Viagra. But here's what else it can do -
- New research suggests intermittent fasting increases the risk of dying from heart disease -
- AFL considers independent doctors at games to help assess head knocks -
- The role of the physiotherapist in concussion in sport -
- Six tips for sticking to your fitness goals -
- How Cold Weather Saps Your Endurance -
- Esports, pickleball and obstacle course racing are surging in popularity - what are their health benefits and challenges? -
- Football codes' lack of response to AIS concussion guidelines leaves players in limbo for 2024 season -
- Insufficient Evidence for Load as the Primary Cause of Nonspecific Chronic Low Back Pain -
- Does playing football really increase the risk of knee osteoarthritis? -
- AFL changes concussion guidelines for community football but elite level protocols stay the same -
- Gabrielle is hesitant to return to sport after an ACL injury -
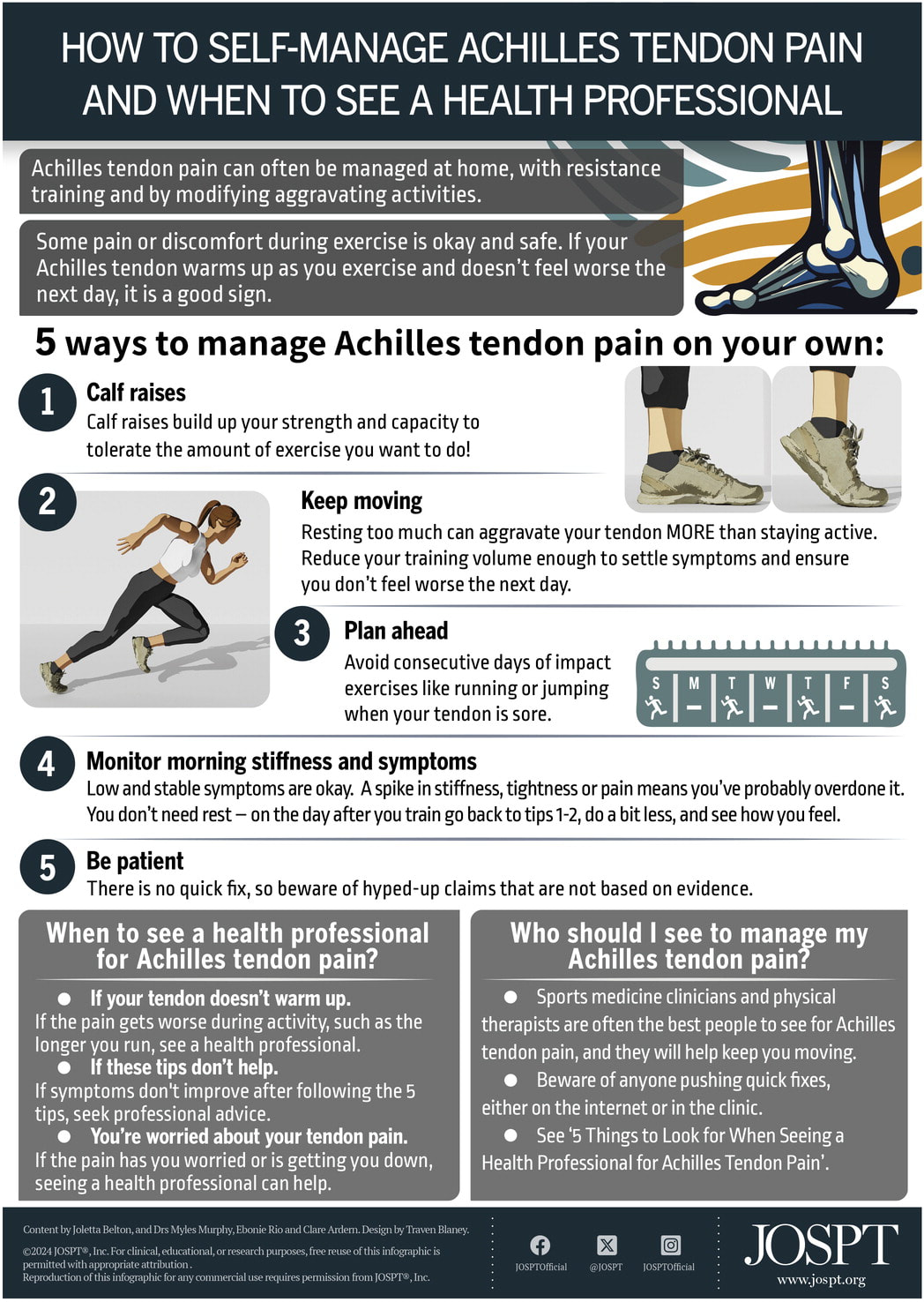
Some pain or discomfort during exercise is OK and safe. It is a good sign if your pain warms up as you exercise and doesn’t feel worse the next day.
KEEP MOVING
Resting too much can be more aggravating than staying active. Reduce your training volume enough to settle symptoms and ensure you don’t feel worse the next day.
PLAN AHEAD
Avoid consecutive days of impact exercise (like running and jumping) if you are sore.
/ Sunday / - / Tuesday / - / Thursday / - / Saturday /
MONITOR MORNING STIFFNESS & SYMPTOMS
Low and stable symptoms are OK. A spike in stiffness, tightness, or pain, means you’ve probably overdone it the day before. You don’t need complete rest. Continue resistance training, do less impact training.
BE PATIENT
There’s no quick fix.
GENERAL HEALTH
We also need to consider general health variables that contribute to recovery:
- Nutrition
- Hydration
- Stress
- Sleep
J Orthop Sports Phys Ther 2024;54(1):95. doi:10.2519/jospt.2023.9001
- Smart mouthguard the new weapon in rugby concussion -
- Athletes struggling with contraceptives and menstrual health as periods remain taboo in sport -
- I want to eat healthily. So why do I crave sugar, salt and carbs? -
- "Naked carbs" and "net carbs" - what are they and should you count them? -
- High Intensity Exercise Can Reverse Neurodegeneration in Parkinson's Disease -
- Inside the brain of a suspected CTE patient -
- Gradual acceptance of concussion risk prompts new reality for Australian sport -
BPPV is caused by a problem with the inner ear, where a small calcium deposit forms and moves with gravity around the different angled canals of the inner ear. BPPV is “positional” as it is triggered by specific head movements, for example, turning your head to the left with rolling over in bed. Symptoms of vertigo are room spinning, disturbed balance, and nausea.
BPPV typically resolves within a few weeks, but can be recurring.
Your GP can give you anti-nausea medication, and Physiotherapists treat BPPV with a sequence of movements and positions, called the Epley Manoeuvre, that uses gravity to re-position the calcium crystals.
A video of the Dix Hallpike test for BPPV is HERE.
Information on the Epley Manoeuvre is HERE.
A video of the Epley Manoeuvre is HERE.
Do you have vertigo? Book a physiotherapy appointment in Mosman to perform the Epley Manoeuvre HERE.
- Can kimchi really help you lose weight? -
- How exercise can treat and prevent common mental health issues -
- Can Strength Training Protect You From Running Injuries? -
- Running or Yoga can help beat depression -
- Many of the supposed benefits of sauna and ice baths are not backed by solid evidence -
- Is it broken? A strain or sprain? How to spot a serious injury -
- How long does back pain last? And how can learning about pain increase the chance of recovery? -
- Concussion in sport: why making players sit out for 21 days afterwards is a good idea -
- How much weight do you actually need to lose? It might be a lot less than you think -
- Fempro Armour looks to minimise sporting injuries among women -
- NRL concussion revolution: Contact training limit on cards -
- How long does low back pain last and what treatments can help? -
- Why the biggest threat to the Matildas' knees is sitting on a plane -
- How women respond to strength training -
Archives
July 2024
June 2024
May 2024
April 2024
March 2024
February 2024
January 2024
December 2023
November 2023
October 2023
September 2023
August 2023
July 2023
June 2023
May 2023
April 2023
March 2023
February 2023
January 2023
December 2022
November 2022
October 2022
September 2022
August 2022
July 2022
June 2022
May 2022
April 2022
March 2022
February 2022
January 2022
December 2021
November 2021
October 2021
September 2021
August 2021
July 2021
June 2021
May 2021
April 2021
March 2021
February 2021
January 2021
December 2020
November 2020
October 2020
September 2020
August 2020
July 2020
June 2020
May 2020
April 2020
March 2020
February 2020
December 2019
November 2019
October 2019
September 2019
August 2019
July 2019
June 2019
May 2019
April 2019
March 2019
January 2019
December 2018
November 2018
October 2018
September 2018
August 2018
July 2018
June 2018
May 2018
April 2018
March 2018
February 2018
January 2018
December 2017
November 2017
October 2017
September 2017
August 2017
July 2017
June 2017
May 2017
April 2017
March 2017
February 2017
January 2017
December 2016
November 2016
May 2016
November 2015
October 2015
September 2015
August 2015
July 2015
June 2015
May 2015
Categories
All
Achilles
ACL
Active Transport
Acupuncture
Ageing
AHPRA
Alcohol
Ankle
Ankylosing Spondylitis
Apps
Arthritis
Arthroscopy
Babies
Backpacks
Back Pain
Blood Pressure
BMI
Body Image
Bunions
Bursitis
Cancer
Chiro
Chiropractic
Cholesterol
Chronic Pain
Concussion
Copenhagen
Costochondritis
Cramp
Crossfit
Cycling
Dance
Dementia
Depression
De Quervains
Diet
Dieting
Elbow
Exercise
Falls
Fat
Feet
Fibromyalgia
Fibula
Finger
Fitness Test
Food
Foot
Fracture
Fractures
Glucosamine
Golfers Elbow
Groin
GTN
Hamstring
Health
Heart-disease
Heart-failure
Heat
HIIT Training
Hip-fracture
Hydration
Hyperalgesia
Ibuprofen
Injections
Injury
Injury Prevention
Isometric Exercise
Knee
Knee Arthroscopy
Knee Replacement
Knees
LARs Ligament Reconstruction
Lisfranc
Load
Low Back Pain
Massage
Meditation
Meniscus
Minimalist Shoes
MRI
MS
Multiple Sclerosis
Netball
Nutrition
OA
Obesity
Orthotics
Osgood-Schlatter
Osteoarthritis
Osteopath
Osteoperosis
Pain
Parkinsons
Patella
Peroneal-tendonitis
Physical-activity
Physio
Physio Mosman
Pigeon-toed
Pilates
Piriformis
Pokemon
Posture
Prehab
Prolotherapy
Pronation
PRP
Radiology
Recovery
Rehab
Rheumatoid
Rheumatoid-arthritis
Rotator Cuff
RTP
Rugby
Running
Running Shoes
Scan
Severs
Shin-pain
Shoes
Shoulder
Shoulder Dislocation
Sitting
Sleep
Soccer
Spinal-fusion
Spondyloarthritis
Spondylolisthesis
Sports Injury
Sports Physio
Standing
Standing-desk
Statins
Stem-cells
Stress Fracture
Stretching
Sugar
Supplements
Surgery
Sweat
Tendinopathy
Tendinosis
Tendonitis
Tmj
Treatment
Vertigo
Walking
Warm-Up
Weight Loss
Wheezing
Whiplash
Wrist
Yoga





















 RSS Feed
RSS Feed