|
Osteoarthritis (OA) is a leading and increasing cause of disability and has a significant impact on health-related quality of life. Osteoarthritis is a structural change to the cartilage and boney surfaces in a synovial joint. Most of the joints in our skeletal system are synovial joints, which is where two opposing bones articulate in a joint capsule filled with synovial fluid. The synovial fluid is a lubricant to help the joint move, as well as a source of nutrition for the cartilage that lines the joint surfaces. The articulating surfaces in synovial joints are lined with articular cartilage, which is a smooth, glossy surface to decrease the friction in the joint (as opposed to fibrous cartilage, which is the rubbery type cartilage that plays a more structural role, found in the meniscus in knees and the rubbery part of your ribs, nose, and ears).
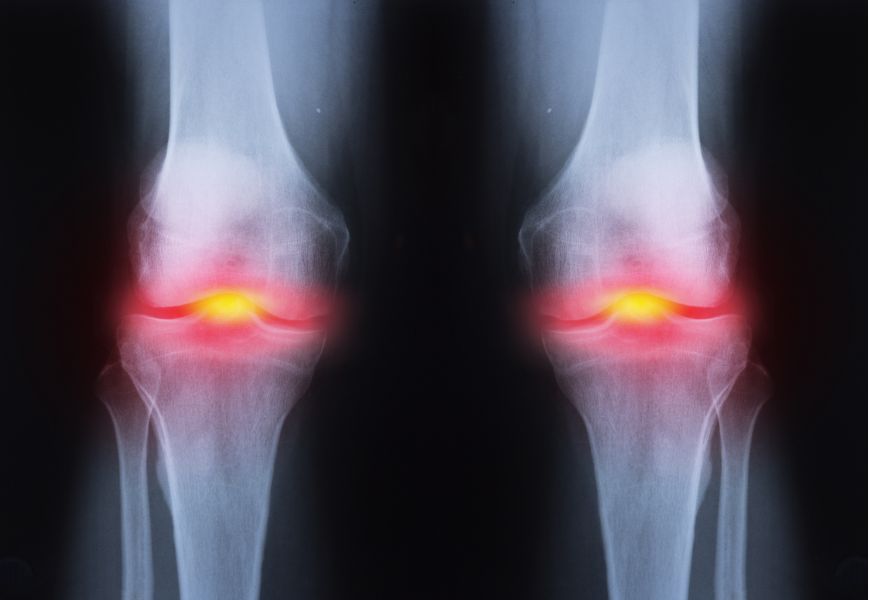
The fleshy parts of muscles and organs is pink because it is full of blood, which brings oxygen and nutrition, and is important for healing damage. Cartilage looks white because it doesn’t have a blood supply, so articular cartilage relies of the synovial fluid for its nutrition. This isn’t as effective as having a blood supply, so when cartilage is damaged it doesn’t heal well. Nanna damages the cartilage in her knees and it never really repairs. Once articular cartilage is damaged, the joint tries to reinforce and repair the damaged area by laying down new tissue. It would be great if cartilage repaired itself with new cartilage cells, but the joint wants to make itself even stronger than the obviously insufficient cartilage, so it lays down a stronger building block - bone cells. So when we say that Nanna has “worn away” her knee to the point where it’s “bone on bone”, it’s not just that she’s warn away the cartilage, but actually there’s also a build up of “extra” bone, as the knee tries to make itself stronger than cartilage. Rather than being a nice smooth, glossy surface, the extra bone is now a bit rough, so we can hear and feel some gravely crunching and creaking in an osteoarthritic joint. Osteoarthritis occurs most frequently in the knees, hips, hands, and spine and is more common the older we get. Osteoarthritis is diagnosed with an X-ray that shows the changes to the bony profile in the joint. When we look at what causes osteoarthritis:
Osteoarthritis isn't painful most of the time. At a certain age, essentially everyone will have arthritic changes in their joints without knowing about it. When we X-ray the joint, it doesn’t look as good as it used to, but it doesn’t hurt. It’s a bit like my grey hair and wrinkles - they don’t look great anymore, and it's a sign that I’m getting older, but I don’t expect them to be painful. If an arthritic joint is painful, it tends to go through phases of being sore and not being sore at all. It can be sore for a day, a week, a month, or a year, but then will be fine again. Whether or not it is sore is not determined by the severity of the changes we see on the X-ray. We can see nasty looking joints that have never been sore, and we see very sore joints that look fine on the X-ray. There isn’t much of a correlation. What determines whether or not the osteoarthritis hurts is the body’s perception of "vulnerability" in that joint - essentially whether or not it feels strong or weak. Pain is an alarm system “software”, employed to defend against damage to the "hardware”. We can have different levels of sensitivity of how easily the alarm is triggered. Very commonly, an arthritic joint starts to hurt more after a period of rest, as the body looses some fitness, muscles loose some strength, an arthritic joint gets less support from the external scaffolding of the muscles, it feels more vulnerable, and communicates that by being painful, as a way of saying “be careful”. So that gives us some treatment options for arthritis: WEIGHT LOSS (Adipose)
EXERCISE
PAIN RELIEF
SURGERY
How do you decide when it’s time to have a joint replacement? I suggest it’s time when you really can’t walk anymore because of the pain, and/or the pain is stopping you sleeping at night. Joint replacements last for about 25 years on average, so don’t rush into doing it too early. The rehab after surgery is 3-12 months before the leg completely feels like it’s yours. The joint replacements are good for relieving pain, but unfortunately we don’t see improvements in patients’ activity levels after surgery. Total hip replacements are easier all around than total knee replacements. Do you have Osteoarthritis? Comments are closed.
|
�
Archives
July 2024
Categories
All
|
|
|
MENU
|
INJURY INFO
|
INJURY INFO
PHYSIO MOSMAN |
Copyright© 2024| Fit As A Physio | ABN 62855169241 | All rights reserved | Sitemap
 RSS Feed
RSS Feed