|
I’ve been treating a chap with a sore knee who really wants to have an arthroscope (keyhole surgery). The knee’s been sore for a while. There’s some “degenerative changes” on a scan, including a torn meniscus. There’s a local knee surgeon who’s really good and is a friend of his. He thinks it’s a no-brainer. He needs an arthroscope. It a quick and easy solution to his problem that has worked well for him and his friends previously. It’s time to have “a bit of a tidy up”. This is a very common presentation, and having an arthroscopic debridement is a very popular decision. 75,000 knee arthroscopies are performed in Australia each year. Therefore, you would imagine there is good evidence to support having one. Unfortunately it depends on who you speak to… A change has been in the air since a 2002 randomised controlled study allocated 180 patients with osteoarthritis to either an arthroscopic “tidy up”, or sham surgery (where the patient was given an anaesthetic, incisions were made, but no actual “tidying up” was done) and the study concluded there was no meaningful difference in pain or function between the groups at follow up. Since then, a number of studies have compared arthroscopic debridements and partial meniscectomy for degenerative knee injuries with exercise or doing nothing (Herrlin 2007, Kirkley 2008, Katz 2013, Sihvonen 2013, Yim 2013, Kise 2016) and the results have been unanimous. A recent systematic review summarises: “these findings do not support the practise of arthroscopic surgery for middle aged or older patients with knee pain, with or without signs of osteoarthritis.” And another: “A trial of nonoperative management should be the first-line treatment for such patients.” Editorials summarise that: “This high quality evidence dictates that meniscectomy is an ineffective treatment for symptomatic degenerative meniscal tears.” And that… “Arthroscopy for degenerative meniscal tears is no longer supported.” (ref) And “There is now overwhelming evidence that arthroscopic knee surgery offers little benefit for most patients with knee pain.” (ref) SO WHY DID THE ARTHROSCOPE WORK FOR ME?We do a lot of arthroscopes and people get better. What’s happening? When you come and see me with degenerative knee pain and I tell you, “you need to do six to twelve weeks of strengthening exercises”, it sounds like hard work. Pffft. Understandably we want an easier option. “Have surgery” sounds like an easier option. Someone else is doing the work for you. After the surgery, you proceed to do six to twelve weeks of strengthening exercises, but this time you’re happier to do the work because we take surgical post-op instructions seriously. Twelve weeks later both these two groups are a lot better. Bingo-bango, “surgery” fixed me. Two million knee arthroscopies a year globally, costing billions of dollars. WHY DO PEOPLE HAVE SURGERY?A pretty typical pathway goes something like:
I think we need to be careful at the MRI stage. MRIs are a lot cheaper and easier to get these days so it’s less of a big deal to get one. I was chatting to a mate with a sore knee and his MRI showed some degenerative changes. Rather than being told that it’s normal to see those sorts of things in knees as old as ours, and that it’s not necessarily the thing that’s giving him pain, he was told the knee is “bone on bone”. How can anyone ever expect to recover without surgery with that sort of imagery? Bone on bone seems definitive. Surely the only way to fix “bone on bone” is surgery? But we know degenerative changes on MRI are poorly associated with symptoms, and degenerative changes are the norm in middle-aged knees (ref). Let’s try some strengthening. You will be surprised. SO WHO SHOULD HAVE SURGERY ON THEIR CARTILAGE?The people I do refer to a surgeon for cartilage surgery have suffered an acute twisting injury with mechanical “locking” symptoms (i.e., an inability to fully extend the painful knee because of a meniscus tear lodged between the articular surfaces).
I had Osgood Schlatter's Disease myself in both knees as a kid. Mum entered some fun-runs in the 80's and we used to go running together. I was training more than I should have for cross-country running in years 5, 6, and 7, and suffered terribly. Terrible night pain - I used to cry. Mum took me to a GP who confirmed the diagnosis with an x-ray and told me to stop running. Crazy sounding diagnosis. It sounded absolutely bizarre to my 10 year old ears. I ran less, and it eventually stopped hurting. I've still got decent bumps on my tibial tubercles to show for it. Osgood-Schlatter's is an overuse injury of the spot where the quadriceps muscle attaches on the front of the knee (tibial tubercle). It’s the tendon where the quads anchors onto the tibia. It get’s sore with too much running, jumping, and kicking. Usually 9-12 year olds. Quite often if they’re having a bit of a growth spurt while they’re doing a lot of training. The body is busy spending its resources on the growing, and so the recovery between training sessions doesn’t keep up.
It’s usually sore after training when you cool down. It can ache in bed at night. We say that it is self-limiting, which means it eventually gets better when you stop growing, but who wants to wait that long? There’s no long-term problems from it. Once it stops hurting it’s all OK. It doesn’t need an x-ray or a scan, or any injections or surgery. It's an easy clinical diagnosis and simple conservative management. DO:
DON’T:
It’s really a matter of adjusting the running load day-to-day depending on how sore it is. If it’s sore - do less. It's an injury that needs managing through the season. I try and get kids to do a bit less running at training and save it for game day. If it's sore on game day and you need to keep playing, it's safe, in that, it's not going to snap or pop. But it will hurt more for longer if you push through, which is what just has to be done some times. Funny sounding name. Not funny at all when it's sore.
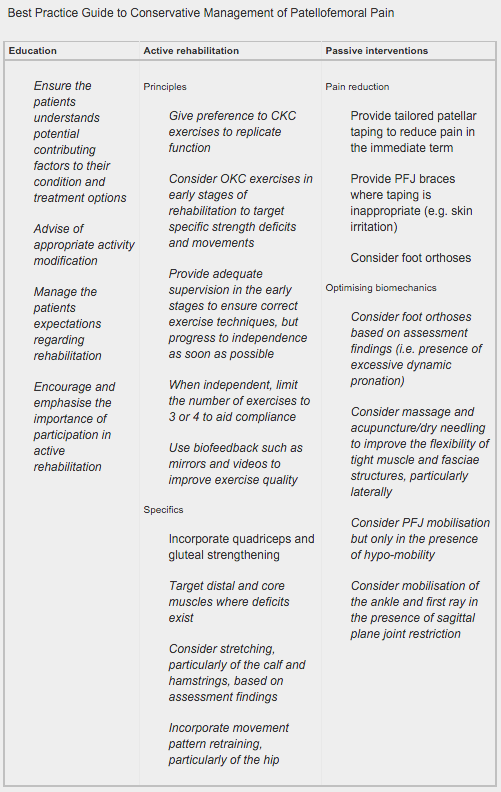
Research Summary: The ‘Best Practice Guide to Conservative Management of Patellofemoral Pain’: incorporating level 1 evidence with expert clinical reasoning (Barton et al, 2015). Patellofemoral pain (PFP) is a common cause for knee pain in general practice and sports settings. Pain is aggravated by running, stairs, and squatting. The majority of suffers report an onset of pain in early adolescence and chronic ongoing pain for up to 20 years. A number of high-quality reviews covering conservative interventions for PFP provide greater guidance for research and clinical practice. Four key principles to ensure effective management include: (1) PFP is a multifactorial condition requiring an individually tailored multimodal approach. (2) Immediate pain relief should be a priority to gain patient trust. (3) Patient empowerment by emphasising active over passive interventions is important. (4) Good patient education and activity modification is essential. Research supports a multimodal treatment approach including:
The ‘Best Practice Guide to Conservative Management of Patellofemoral Pain’ has been based on a combination of contemporary level 1 evidence and the analysis of international experts’ clinical reasoning: ACL Rehabilitation Guide (available here) A criteria driven ACL rehabilitation protocol and guide for both clinicians and people who have undergone a surgical reconstruction of the Anterior Cruciate Ligament (ACL). Author: Randall Cooper
Netball Australia has developed a great program to help prevent knee and other lower limb injuries in netball.
Knee and ankle injuries are common in netball, making up three quarters of all injuries. Devastating ACL injuries are unfortunately common, making up 25% of serious injuries. The KNEE program offers a range of warm-up exercises that help prevent injury. There are a range of age and experience appropriate exercises for junior through to elite netballers. They are easily understood by players and coaches, with a number of options offering variability and progression. It would be great to see this program widely adopted by Australia's largest participation sport for females. |
�
Archives
July 2024
Categories
All
|
|
|
MENU
|
INJURY INFO
|
INJURY INFO
PHYSIO MOSMAN |
Copyright© 2024| Fit As A Physio | ABN 62855169241 | All rights reserved | Sitemap



 RSS Feed
RSS Feed