|
Sydney is in lockdown again from Friday June 25th to Friday July 9th.
During this current lockdown, Fit As A Physio is staying open to continue offering quality care to my clients. The Department of Health has specifically confirmed that physiotherapy is deemed an essential service. The Health Minister has encouraged private practices to remain open, as it will reduce demand on general practice and the hospitals if patients can still see their physiotherapist for their musculoskeletal and acute care management. I have completed the Department of Health's "COVID-19 Infection Control Training". I have reviewed all clinic hygiene practices, to ensure optimal safety and care for every person who attends the clinic. There are many things I am doing as a registered health professional to minimise risk of exposure, through rigorous hygiene practices, and patient screening, to keep you safe. You are welcome to attend your appointment, subject to the following conditions:
Thank you for your cooperation with these measures. For our safety:
If you are in self-isolation or would prefer to minimise contact in any way, you may like to consult with me via video. "Telehealth" uses technology that’s readily available on your computer or phone to receive assessment, diagnosis, and rehab prescription. FaceTime, Skype, or PhysiApp are easy options. The standard consultation via telehealth is $39/15mins. If you would like to talk to me about commencing or continuing your physio through Telehealth, please phone 9969 6925, email fergus@fitasaphysio.com, or book online here. Stay safe and well. Kind regards, Fergus Tilt Sports & Exercise Physiotherapist Fit As A Physio | MOSMAN
0 Comments
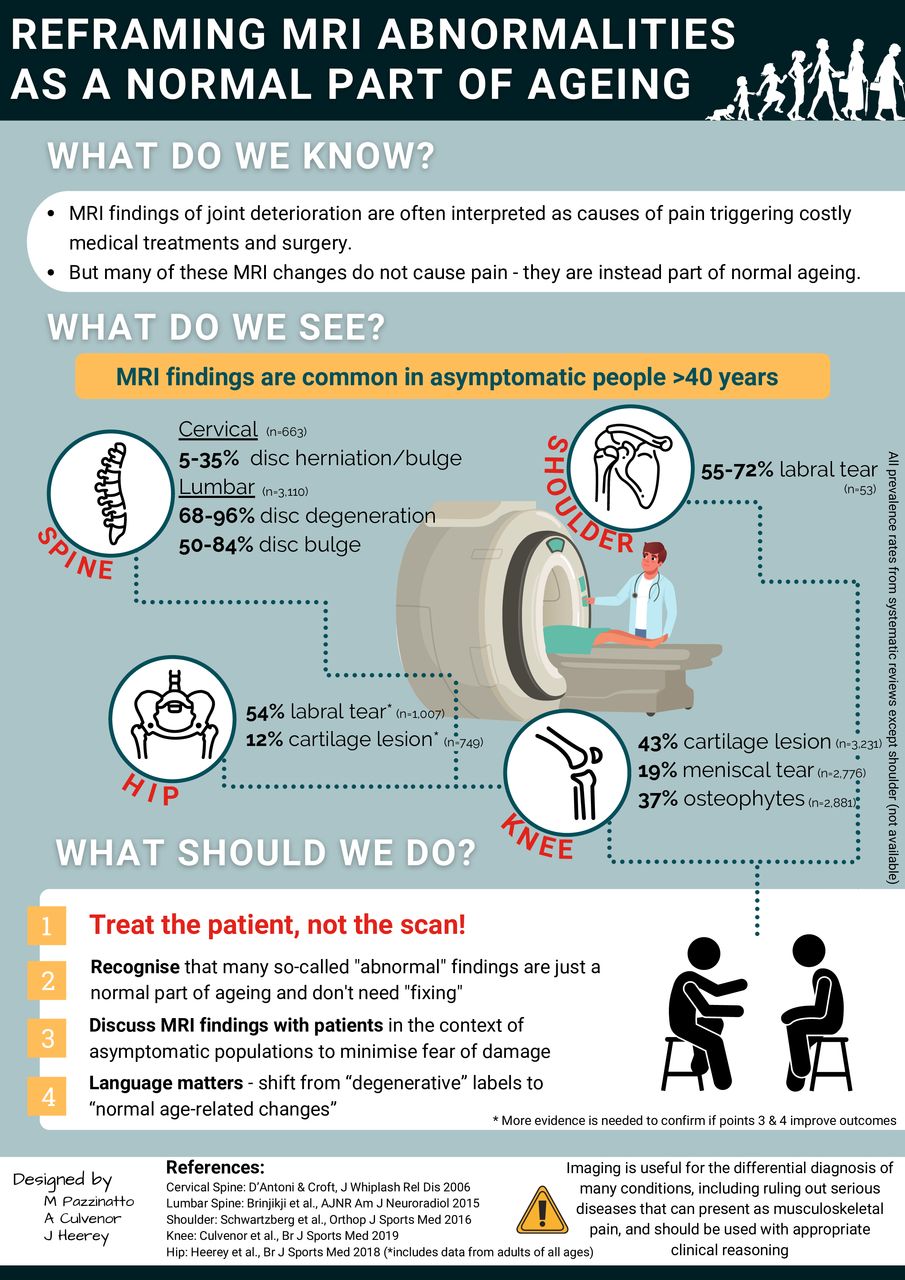
Sports and exercise medicine clinicians often refer for diagnostic imaging to help direct clinical management. The use of musculoskeletal MRI has risen rapidly in recent decades, yet the clinical benefit of MRI is uncertain. Imaging is useful for the differential diagnosis of many health conditions, including possible red flags, however, there are growing concerns of potential harm from MRIs caused by clinicians misinterpreting results triggering unnecessary interventions escalating patient fear/distress. Evidence-based reporting and clinically relevant interpretation of MRIs is critical.
Recognising the clinical significance of MRI findings is often a challenge given the substantial discordance that exists between structural pathology and symptoms. Emerging evidence indicates a high prevalence of so-called abnormal findings on MRI in individuals without symptoms. A collation of systematic reviews (and cohort studies when no review available) highlights that typical features of deterioration, such as cartilage lesions, hip and shoulder labral tears and spinal changes (eg, disc degeneration/bulge) exist in many healthy asymptomatic adults (figure 1). Approximately 8 of 10 adults aged ≥40 years have asymptomatic disc degeneration, while almost half of all adults aged ≥40 years have knee cartilage lesions but no pain. Although the prognosis of these asymptomatic findings is not well established, even in cases of further structural deterioration (eg, longitudinal cartilage loss) the association with pain appears minimal.5 These findings are critical for clinicians and patients to understand the relevance of structural pathology and can be used to address recent calls for radiology reports to include age-matched asymptomatic prevalence rates. Such an approach, together with discussion with patients putting MRI findings into context, may help minimise patient anxiety, and beliefs they are damaged and vulnerable, as a result of a diagnostic label. Including such epidemiological information on spinal MRI reports reduced subsequent opioid prescription although had little effect on healthcare utilisation. The high prevalence of asymptomatic changes on MRI emphasises that such features may not always be the source of pain in symptomatic patients and should not routinely be considered as pathological processes requiring intervention. Instead, in many people they likely represent part of the normal ageing process—like wrinkles on the skin. Current evidence suggests that it is more common than not to have a cartilage lesion or disc bulge as we age. Perhaps it is time we redefine what a ‘normal’ MRI is and start being ‘CLEAR’ with patients when discussing imaging results—consistent language, including epidemiological information and assessment of relevance.
|
�
Archives
April 2024
Categories
All
|
|
|
MENU
|
INJURY INFO
|
INJURY INFO
PHYSIO MOSMAN |
Copyright© 2024| Fit As A Physio | ABN 62855169241 | All rights reserved | Sitemap



 RSS Feed
RSS Feed