HEEL PAIN IN CHILDREN
Sever’s is most common in 9 - 12 year olds. It’s sore to squeeze the bone at the base of the Achilles where it attaches onto the heel. It’s not something that can be seen - it never seems to look red or swollen. It’s worse after sprinting, jumping, and hopping. It settles with rest. It is an overuse injury so it’s common in pre-season, or anytime training loads increase too quickly. My kids get it when they do extra sessions in running spikes or footy boots, without the normal heel support of their running shoes. It’s an overuse injury from excessive loads.
OVERUSE INJURY
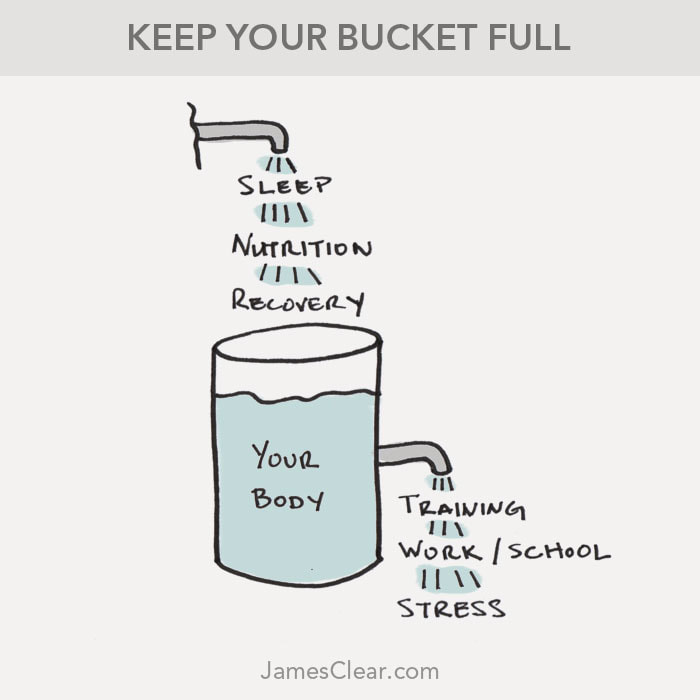
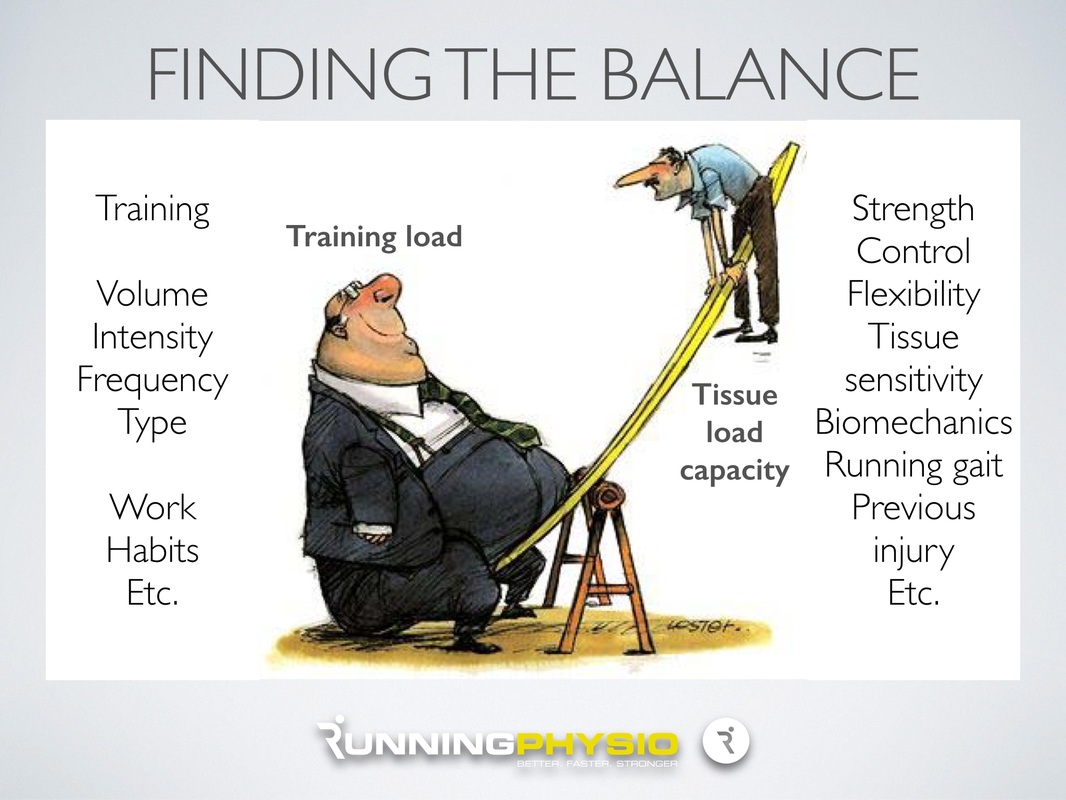
When we talk about excessive loads it can be “external” load such as:
I think the running pace is the more powerful multiplier in this list. Extra sprint sessions will do it. My kids got sore once when we did a boot-camp session with a novel plyometric exercise - split jumps. There are also “internal” variables that determine our ability to cope with the training load:
My kids definitely are more prone to Sever’s if they’ve had a couple of late nights that week. And, if they’re having a growth spurt, their bodies are busy spending resources on growing rather than recovering from the stress of a training session. NATURAL RECOVERY
Text books say that Sever’s disease is self-limiting because the growth plate eventually fuses by the age of 15 or 16. But I don’t think there’s anyone who would be happy to just let it run its course until then. It is usually sore enough to stop you participating in sport, so it needs treatment.
WHAT DO WE DO?
I used to put kids with heel pain in orthotics, until I read this research which confirms that a simple heel wedge is more effective than orthotics for Sever’s disease.
I get them to do an isometric Achilles strengthening program which also helps with pain control. But ultimately recovery comes down to load management. Load management means reducing the excessive loads. So this could be:
And aid recovery with:
With these type of overuse injuries, I interpret "soreness" as essentially the same thing as "tiredness". If they've been training more, sleeping less, or growing more, we would expect some "tiredness". If they were tired what would be the treatment?... Sleep more and train a bit less.
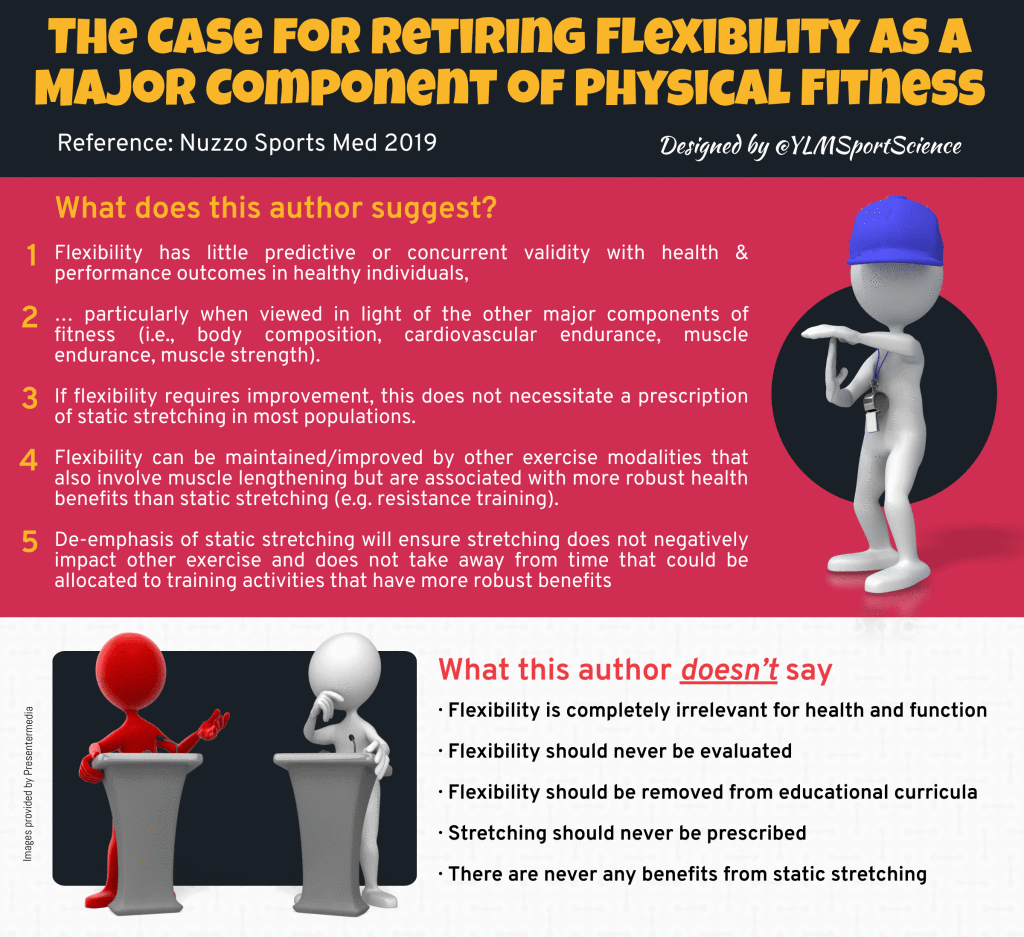
I’d guess that most people feel guilty about not stretching enough. Interestingly, health professionals have changed our tune about the importance of stretching. Research over the last 15 years has suggested static stretching is not as beneficial as was once thought. I’ve been having conversations about the reasons to stretch (or not) for at least the last 15 years, but the current science on stretching just isn’t catching on. So, what do we know?… DOES STRETCHING PREVENT INJURIES? No. There is a lot of evidence that stretching does not reduce the risk of injury. This systematic review and meta-analysis of randomised controlled trials found stretching does not prevent injuries, whether done before or after training. This randomised controlled trial, and this systematic review concluded stretching before exercising only reduces the risk of injury by less than 1%. Therefore, in practical terms the average athlete would need to stretch for 23 years to prevent one injury. Definitely not worth it. DOES STRETCHING HELP MUSCLE SORENESS?No. A systematic review concluded that stretching before or after exercising does not confer protection from muscle soreness (ref). Stretching was found to reduce muscle soreness by a trivially small amount - less than 2%. “Most athletes will consider effects of this magnitude too small to make stretching to prevent later muscle soreness worthwhile.” DOES STRETCHING INCREASE RANGE OF MOVEMENT?No. Stretching for the amount of time that most people would hold their stretches, does not make any actual difference to flexibility. The mechanisms of stretching have been extensively studied. There is moderate evidence from a systematic review that stretching can increase flexibility (ref). However, to achieve an actual improvement in muscle compliance we know the total duration of stretching needs to be at least five minutes per muscle group (ref). Therefore to stretch hamstrings, quads, and calves, both left and right, as part of a warm up before sport, it should take at least 30 minutes - which is practically impossible as part of a warm up. We know the one or two, thirty second stretches the majority of athletes would perform during their warm up are just not enough to actually improve their flexibility (ref). DOES STRETCHING HELP PERFORMANCE?What people find most surprising about static stretching is it impairs subsequent performance (ref). A substantial body of research has shown that sustained static stretching acutely decreases muscle strength and power (ref). Stretching before an endurance event lowers endurance performance and increases the energy cost of running (ref). Cycling efficiency and time to exhaustion are reduced after static stretching (ref). Pretty much any measure of performance is made worse by stretching. Static stretching impairs:
A comprehensive review (ref) from 2011 concludes: “Based on the majority of the literature, it would seem logical to recommend that prolonged static stretching not be performed prior to a high level or competitive athletic or training performance.” WHAT ABOUT DYNAMIC STRETCHING?Obviously, I’ve been talking about sustained, static stretching. It has been shown that there is no stretch-induced strength loss with dynamic stretching (ref). However, the efficacy of dynamic stretching for increasing flexibility is yet to be determined (ref). SO WHY STRETCH?I do get people to stretch if there’s a specific pathology that needs treating. And you do need to stretch if you need flexibility to achieve certain positions in your sporting performance (hurdlers / gymnasts / divers, etc). SO SHOULD WE STOP STRETCHING?If you’re happy with your stretching routine, keep doing it. If you think it feels good to stretch after exercise then there’s no harm. But I definitely wouldn’t recommend stretching at the expense of other techniques that are proven to aid recovery.
TENDON PAIN
Tendinopathy (tendon pain) is very common. They are the most common type of overuse injury (ref). Achilles tendinopathy affects the majority of runners (ref) and is the reason 16% of athletes have to stop sports participation (ref).
There are a range of commonly prescribed treatment options for tendinopathy, but very few are supported by quality, randomised, prospective, placebo-controlled trials. SO WHAT DO I DO?
Considering all the available treatment options, above anything else, I always recommend:
WHAT ABOUT INJECTIONS?
Having mapped out a management plan, patients will routinely ask my opinion on getting an injection. They may have had a friend for whom an injection worked well, or the GP has suggested it as an option, or they’ve had one before and it worked.
There are a range of drugs to inject into or around a tendon, depending on who you are referred to:
CORTICOSTEROIDS
Corticosteroids are an anti-inflammatory medication injected around the tendon to decrease pain that is caused by inflammation (although it is now thought that inflammation does not play a significant role in tendon pain). Corticosteroid injections have historically been commonly prescribed but more recently their use is controversial. Repeated corticosteroid injections can weaken the tendon and increase the risk of rupture. Corticosteroid injections are good at relieving pain in the short term (2-6 weeks) however, there is strong evidence that long-term outcomes (> 6 months) are worse than other conservative treatments or no treatment at all (ref).
"The best systematic review evidence shows that local corticosteroid injections are not effective for tendinopathies after the first few weeks, and produce worse long-term outcomes compared to other treatments" (ref) PROLOTHERAPY / SCLEROTHERAPY
Prolotherapy injections act as an irritant causing an inflammatory response then scarring of the nerves that transmit pain. There is no solid support in the medical literature for this procedure for the treatment of tendinopathies. A randomised controlled trial of polidocanol injections showed the potential to reduce tendon pain in patients with chronic painful mid-portion Achilles tendinopathy (ref). However, a systematic review found limited results for use of prolotherapy in sports related soft tissue injuries (ref).
AUTOLOGOUS BLOOD INJECTIONS
The rationale of autologous blood injection consists of enhancing tendon healing through collagen regeneration and the provision of cellular mediators. Good experimental models are lacking, and clinical application is anecdotal. A 2013 randomised controlled trial investigating the efficacy of autologous blood injections as a treatment for mid-portion Achilles tendinopathy concluded they did not reduce pain or improve function any more than a strengthening program. (ref)
HIGH-VOLUME INJECTIONS
The suggested mechanism of high-volume injections is the mechanical disruption of local tissues then stimulates a healing response. One study (ref) has shown that high-volume injection of normal saline solution, corticosteroids or anaesthetics reduces pain and improves short and long-term function in patients with Achilles tendinopathy. However, more research is required.
PLATELET RICH PLASMA (PRP)
Platelets are naturally occurring in your blood, where they play an important role in healing damaged tissue, so superficially it’s inherently appealing to just add more of them to the sore spot. PRP injections are particularly trendy at the moment and it’s easy to find someone who will tell you they work well. Unfortunately, research concludes there is no benefit to PRP injections. This study found PRP injections do not improve plantar fasciopathy pain or function. This study concluded there is insufficient evidence to support the use of PRP for treating musculoskeletal soft tissue injuries. This systematic review found strong evidence against platelet-rich plasma injections for tennis elbow. This study found PRP did not improve tendon structure. This meta-analysis found no greater clinical benefit of PRP over placebo or dry needling for tendinopathy.
SO…
Would I have any of these injections, or would I recommend them to my patients, friends, or family? Well it depends. In my experience some people get some benefit some of the time. HOWEVER, these injectables are not consistently effective and their use is mostly not supported by research. I suggest that patients try the strengthening program and the results will be overall better in the long term.
WHY DO THE INJECTIONS WORK FOR SOME PEOPLE?
I’ve been frustrated with a couple of patients that cancelled their follow-up appointment and, when I phoned and asked what had happened, they’ve had an injection and now feel fine. My conclusion is the injections don’t work, but if you were sore and now you’re not, your conclusion would be they do work. So what is it?..
REGRESSION TO THE MEAN
Most people seek treatment when they are at their worst. By definition the only possible change from being as bad as at can be, is an improvement. Was it the injection working, or was it getting better anyway?
NATURAL HISTORY
Some conditions are self limiting and will just get better by themselves. Did the injection work, or was it about to get better anyway?
PLACEBO
SUMMARY
I understand that getting an injection seems like a much easier option than doing 12-weeks of strengthening exercises, but in the long run, a strengthening program is the thing that actually works.
TL;DR
If treating tendon pain was as easy as getting an injection then that’s what everyone would do first. Unfortunately it’s not as easy as that.
Adaptations to TrainingWhen we “use” our bodies, our bodies adapt to the activity we are doing. The more we do, the more we are able to do. The less we do, the less we are able to do. This is essential in eliciting a training response. When we train we want to cause stress to our body. (This may be our muscles, bones, cardiovascular system, etc.) We want to overload the system, which causes a degree of damage or micro-trauma. The body then responds by growing bigger / stronger / faster / fitter, so it can cope with that load in future. We cause stress to force adaptations. Stress/load => damage => rest/recovery => adaptation/growth. LoadA lot of common gradual-onset injuries result from a failure to adapt to load. There are a number of variables that can be multiplied to determine the total load:
The intensity of the activity is the most powerful multiplier in this list. When we are considering total load, we also need to consider variables that make it harder for our bodies to adapt to load. Variables that can be multiplied to determine how well we adapt to the load:
Recent research found that getting less than 8 hours sleep a day almost doubles the injury rate in athletes.
|
�
Archives
July 2024
Categories
All
|
|
|
MENU
|
INJURY INFO
|
INJURY INFO
PHYSIO MOSMAN |
Copyright© 2024| Fit As A Physio | ABN 62855169241 | All rights reserved | Sitemap









 RSS Feed
RSS Feed