|
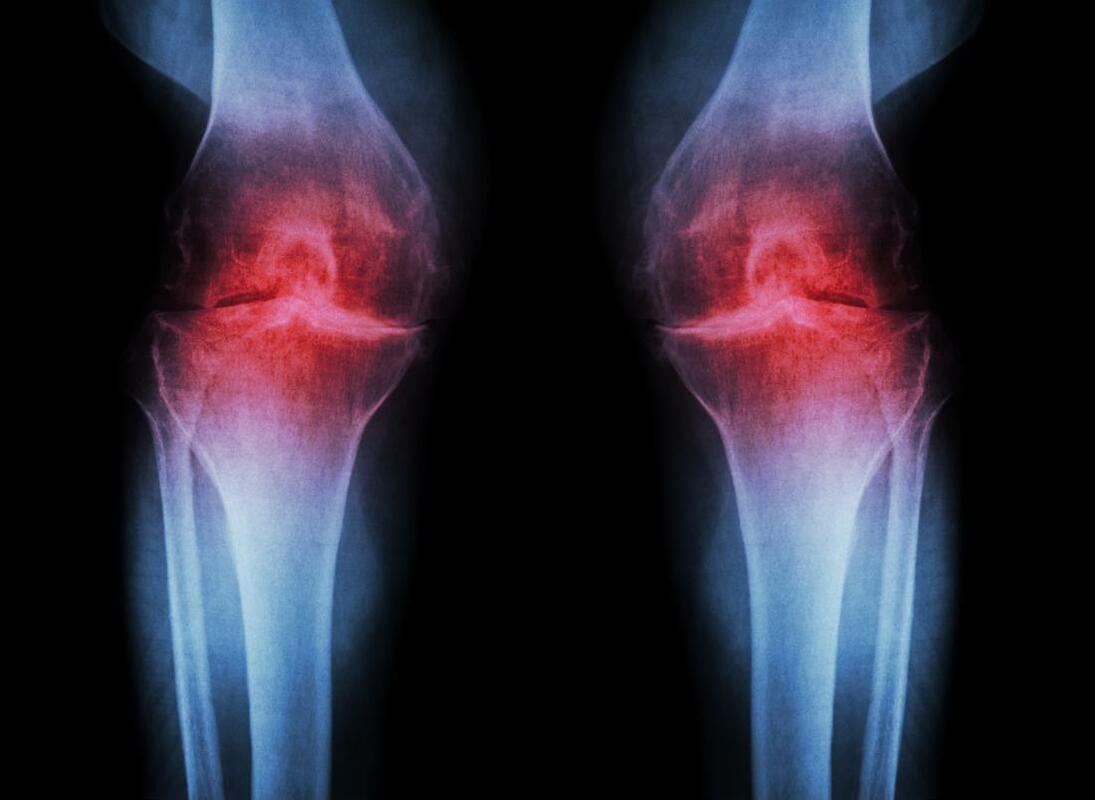
Osteoarthritis (OA) is a leading and increasing cause of disability and has a significant impact on health-related quality of life. Osteoarthritis is a structural change to the cartilage and boney surfaces in a synovial joint. Most of the joints in our skeletal system are synovial joints, which is where two opposing bones articulate in a joint capsule filled with synovial fluid. The synovial fluid is a lubricant to help the joint move, as well as a source of nutrition for the cartilage that lines the joint surfaces. The articulating surfaces in synovial joints are lined with articular cartilage, which is a smooth, glossy surface to decrease the friction in the joint (as opposed to fibrous cartilage, which is the rubbery type cartilage that plays a more structural role, found in the meniscus in knees and the rubbery part of your ribs, nose, and ears).
The fleshy parts of muscles and organs is pink because it is full of blood, which brings oxygen and nutrition, and is important for healing damage. Cartilage looks white because it doesn’t have a blood supply, so articular cartilage relies of the synovial fluid for its nutrition. This isn’t as effective as having a blood supply, so when cartilage is damaged it doesn’t heal well. Nanna damages the cartilage in her knees and it never really repairs. Once articular cartilage is damaged, the joint tries to reinforce and repair the damaged area by laying down new tissue. It would be great if cartilage repaired itself with new cartilage cells, but the joint wants to make itself even stronger than the obviously insufficient cartilage, so it lays down a stronger building block - bone cells. So when we say that Nanna has “worn away” her knee to the point where it’s “bone on bone”, it’s not just that she’s warn away the cartilage, but actually there’s also a build up of “extra” bone, as the knee tries to make itself stronger than cartilage. Rather than being a nice smooth, glossy surface, the extra bone is now a bit rough, so we can hear and feel some gravely crunching and creaking in an osteoarthritic joint. Osteoarthritis occurs most frequently in the knees, hips, hands, and spine and is more common the older we get. Osteoarthritis is diagnosed with an X-ray that shows the changes to the bony profile in the joint. When we look at what causes osteoarthritis:
Osteoarthritis isn't painful most of the time. At a certain age, essentially everyone will have arthritic changes in their joints without knowing about it. When we X-ray the joint, it doesn’t look as good as it used to, but it doesn’t hurt. It’s a bit like my grey hair and wrinkles - they don’t look great anymore, and it's a sign that I’m getting older, but I don’t expect them to be painful. If an arthritic joint is painful, it tends to go through phases of being sore and not being sore at all. It can be sore for a day, a week, a month, or a year, but then will be fine again. Whether or not it is sore is not determined by the severity of the changes we see on the X-ray. We can see nasty looking joints that have never been sore, and we see very sore joints that look fine on the X-ray. There isn’t much of a correlation. What determines whether or not the osteoarthritis hurts is the body’s perception of "vulnerability" in that joint - essentially whether or not it feels strong or weak. Pain is an alarm system “software”, employed to defend against damage to the "hardware”. We can have different levels of sensitivity of how easily the alarm is triggered. Very commonly, an arthritic joint starts to hurt more after a period of rest, as the body looses some fitness, muscles loose some strength, an arthritic joint gets less support from the external scaffolding of the muscles, it feels more vulnerable, and communicates that by being painful, as a way of saying “be careful”. So that gives us some treatment options for arthritis: WEIGHT LOSS (Adipose)
EXERCISE
PAIN RELIEF
SURGERY
How do you decide when it’s time to have a joint replacement? I suggest it’s time when you really can’t walk anymore because of the pain, and/or the pain is stopping you sleeping at night. Joint replacements last for about 25 years on average, so don’t rush into doing it too early. The rehab after surgery is 3-12 months before the leg completely feels like it’s yours. The joint replacements are good for relieving pain, but unfortunately we don’t see improvements in patients’ activity levels after surgery. Total hip replacements are easier all around than total knee replacements. Do you have Osteoarthritis?
0 Comments
I’ve been treating a chap with a sore knee who really wants to have an arthroscope (keyhole surgery). The knee’s been sore for a while. There’s some “degenerative changes” on a scan, including a torn meniscus. There’s a local knee surgeon who’s really good and is a friend of his. He thinks it’s a no-brainer. He needs an arthroscope. It a quick and easy solution to his problem that has worked well for him and his friends previously. It’s time to have “a bit of a tidy up”.
This is a very common presentation, and having an arthroscopic debridement is a very popular decision. 75,000 knee arthroscopies are performed in Australia each year. Therefore, you would imagine there is good evidence to support having one. Unfortunately it depends on who you speak to…
A change has been in the air since a 2002 randomised controlled study allocated 180 patients with osteoarthritis to either an arthroscopic “tidy up”, or sham surgery (where the patient was given an anaesthetic, incisions were made, but no actual “tidying up” was done) and the study concluded there was no meaningful difference in pain or function between the groups at follow up. Since then, a number of studies have compared arthroscopic debridements and partial meniscectomy for degenerative knee injuries with exercise or doing nothing (Herrlin 2007, Kirkley 2008, Katz 2013, Sihvonen 2013, Yim 2013, Kise 2016) and the results have been unanimous. A recent systematic review summarises: “these findings do not support the practise of arthroscopic surgery for middle aged or older patients with knee pain, with or without signs of osteoarthritis.” And another: “A trial of nonoperative management should be the first-line treatment for such patients.”
Editorials summarise that:
“This high quality evidence dictates that meniscectomy is an ineffective treatment for symptomatic degenerative meniscal tears.”
And that… “Arthroscopy for degenerative meniscal tears is no longer supported.” (ref) And “There is now overwhelming evidence that arthroscopic knee surgery offers little benefit for most patients with knee pain.” (ref) SO WHY DID THE ARTHROSCOPE WORK FOR ME?
We do a lot of arthroscopes and people get better. What’s happening?
When you come and see me with degenerative knee pain and I tell you, “you need to do six to twelve weeks of strengthening exercises”, it sounds like hard work. Pffft. Understandably we want an easier option. “Have surgery” sounds like an easier option. Someone else is doing the work for you. After the surgery, you proceed to do six to twelve weeks of strengthening exercises, but this time you’re happier to do the work because we take surgical post-op instructions seriously. Twelve weeks later both these two groups are a lot better. Bingo-bango, “surgery” fixed me. Two million knee arthroscopies a year globally, costing billions of dollars. WHY DO PEOPLE HAVE SURGERY?
A pretty typical pathway goes something like:
I think we need to be careful at the MRI stage. MRIs are a lot cheaper and easier to get these days so it’s less of a big deal to get one. I was chatting to a mate with a sore knee and his MRI showed some degenerative changes. Rather than being told that it’s normal to see those sorts of things in knees as old as ours, and that it’s not necessarily the thing that’s giving him pain, he was told the knee is “bone on bone”. How can anyone ever expect to recover without surgery with that sort of imagery? Bone on bone seems definitive. Surely the only way to fix “bone on bone” is surgery? But we know degenerative changes on MRI are poorly associated with symptoms, and degenerative changes are the norm in middle-aged knees (ref). Let’s try some strengthening. You will be surprised. SO WHO SHOULD HAVE SURGERY ON THEIR CARTILAGE?
The people I do refer to a surgeon for cartilage surgery have suffered an acute twisting injury with mechanical “locking” symptoms (i.e., an inability to fully extend the painful knee because of a meniscus tear lodged between the articular surfaces).
PT Inquest, my favourite physio podcast, recently discussed this paper: The abstract summarises: In contrast to best practice guidelines for knee osteoarthritis (OA), findings from several different healthcare settings have identified that nonsurgical treatments are underused and Total Knee Replacement surgery is overused. Empirical evidence and qualitative observations suggest that patients’ willingness to accept nonsurgical interventions for knee OA is low. Participants’ beliefs about knee OA and its treatment were identified. Beliefs were grouped into five belief dimensions:
The participants' beliefs are what I would guess, based on what I hear from patients everyday:
The authors conclude: Common misconceptions about knee OA appear to influence patients’ acceptance of nonsurgical, evidence-based treatments such as exercise and weight loss. Once the participants in this study had been “diagnosed” with “bone-on-bone” changes, many disregarded exercise-based interventions which they believed would damage their joint, in favor of alternative and experimental treatments, which they believed would regenerate lost knee cartilage. These misconceptions do feel like commonsense and, as such, are widely held by the general public. Some of them may be true at the very end stage of osteoarthritic disease, but they are definitely not true for all patients with osteoarthritis, and as such, the misconceptions are harmful because patients disregard beneficial conservative treatments like weight loss and exercise, and rush towards surgical options. "BONE ON BONE" is a metaphor that is commonly used, even by physios and knee surgeons. "Bone on bone" creates a very dramatic image of what's going on in the knee, and undermines the possibility of osteoarthritis being pain free. Using words like "bone on bone" can cause harm because it sounds like it is definitive and painful, when in reality it's only a metaphor. The reality could be explained more like: "the joint reinforces and repairs the damaged area by laying down new tissue". Or, "the joint wants to make itself even stronger than cartilage, so it lays down stronger building blocks - bone cells". Not everyone with osteoarthritis has "bone on bone", and the perception of "bone on bone" as what's happening in the knee can make patients less likely to stick with evidence-based conservative treatment options. The concept of "WEAR AND TEAR" makes sense if you imagine the joint as mechanical. A cupboard's metal hinge can be opened and closed a certain number of cycles before it breaks. Metal and plastic fatigues and fails. Mechanical joints "wear out". But our joints aren't made of metal and plastic. Knees are not mechanical joints. They are biologically active joints, that adapt to what we do. If we do a million bicep curls, we don't expect our biceps to "wear out" - we expect to end up with bigger, stronger biceps. Similarly, the bones, cartilage, ligaments and muscles in our knees are biologically adaptive, they have regenerative ability, and adapt to what we do. Our joints get stronger with use. Rather than "wear and tear", the more appropriate phrase should be: "use it or lose it". DOESN'T RUNNING "WEAR OUT" KNEES?Another common misconception is that running "wears out" knees. Doctors and knee surgeons see patients complaining they have sore knees when they run. The X-ray shows some arthritis, so it's very easy to make the assumption that running causes arthritis. But we know that distance runners don't "wear out" their knees. Runners have better knees than non-runners. This 2017 research comparing 2,637 runners to non-runners (matched for age, weight, mileage, injury, and other variables) concludes: There is no increased risk of symptomatic knee OA among runners compared with non-runners. In those without OA, running is not detrimental to the knees. This 2008 research concludes: Long-distance running among healthy older individuals was not associated with accelerated radiographic OA, and long-distance running or other routine vigorous activities should not be discouraged among healthy older adults out of concern for progression of knee OA. This 2004 research concludes: The results of this literature review strongly suggest that regular mild-moderate impact exercise does not increase the risk of OA, and that there is some evidence that it does not increase symptoms in patients with mild-moderate OA. And: Regular running increases joint space width. So:
A systematic review and meta-analysis published in the British Journal of Sports Medicine has concluded PRP injections for osteoarthritis of the knee reduce pain and improve function when compared with placebo injections and hyaluronic acid injections.
However the results should be regarded with caution as almost all the analysed trials included a high risk of bias. Therefore further research is required. |
�
Archives
April 2024
Categories
All
|
|
|
MENU
|
INJURY INFO
|
INJURY INFO
PHYSIO MOSMAN |
Copyright© 2024| Fit As A Physio | ABN 62855169241 | All rights reserved | Sitemap












 RSS Feed
RSS Feed